We all have medical questions that we want answered – that’s why Dr. Amna Asif is here to provide us with her expert opinion! Every other week, she will be sharing her expert advice with us regarding a range of topics our followers are interested in learning more about. This week in Doc Talk, she talks about anaemia, otherwise known as iron deficiency. Read ahead to find out what exactly it is, what the causes and symptoms are, and what you can do to prevent it:
What Is Anaemia?
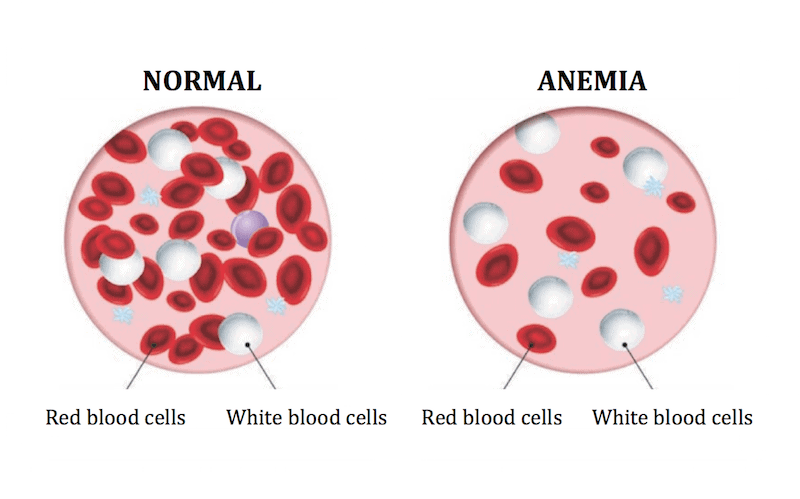
Anaemia is the deficiency of red blood cells or haemoglobin in the body. Red blood cells and haemoglobin, the molecule in red blood cells that makes them red, are important because they carry oxygen from the lungs, around the body.
Anaemia isn’t a disease in itself, but a result of a malfunction somewhere in the body; it’s important to find and treat the cause of the anaemia.
When a person has anaemia, their heart has to work harder to pump the quantity of blood needed to get enough oxygen around their body. During heavy exercise, the cells may not be able to carry enough oxygen to meet the body’s needs and the person can become exhausted and feel unwell.
This condition is common, particularly in females. Some estimates suggest that around 1 in 5 menstruating women, and half of all pregnant women are anaemic.
What Do Red Blood Cells (RBCs) Do?
Red blood cells are produced in the bone marrow and have a lifespan of about 120 days. Millions of new RBCs enter the bloodstream each day in a healthy person. You need certain nutrients in your diet to make and maintain RBCs. Each RBC contains a protein called haemoglobin. This protein gives red blood cells their colour.
Oxygen molecules absorbed in the lungs attach themselves to haemoglobin, which is then delivered to all parts of the body. All of the body’s cells need oxygen to live and perform their various duties.
What Causes Anaemia?
Anaemia can have many causes:
- Dietary deficiency – lack of iron, vitamin B12 or folic acid in the diet.
- Malabsorption – when the body is unable to properly absorb the nutrients in the diet, caused by conditions such as coeliac disease.
- Inherited disorders – such as thalassaemia or sickle cell disease.
- Autoimmune disorders – such as autoimmune haemolytic anaemia.
- Chronic diseases – such as diabetes, rheumatoid arthritis and TB.
- Hormonal disorders – such as hypothyroidism.
- Bone marrow disorders – such as cancer.
- Blood loss – due to trauma, surgery, peptic ulcer, heavy menstruation, cancers or frequent blood donations.
- Drugs and medications – including alcohol, antibiotics, anti-inflammatory drugs or anticoagulant medications.
- Mechanical destruction –mechanical heart valves can damage red blood cells.
- Infection – such as malaria and sepsis.
- Periods of rapid growth or high energy requirements – such as puberty or pregnancy.
What Are The Symptoms?
If you have anaemia, you can experience a range of symptoms:
- Tiredness
- Pale skin
- Rapid or irregular heart beat
- Dizziness or light-headedness
- Shortness of breath, even on mild exertion
- Concentration difficulties
- Cracked or red tongue
- Strange food cravings
- Cold feet or hands
It’s important that you see your doctor if you have any of these symptoms.
People At High Risk Of Anaemia
Certain groups are at increased risk of anaemia:
- Menstruating women
- Pregnant & breastfeeding women
- Babies – especially premature
- Children going through puberty
- People on vegetarian or vegan diet
- People with cancer, stomach ulcers or chronic diseases e.g
- Athletes
- People on fad diets
How Is It Diagnosed?
Depending on the cause, anaemia is diagnosed using a number of tests including:
- Medical history – including any chronic illnesses and regular medication.
- Physical examination – to look for signs of anaemia and a cause for anaemia.
- Blood tests – including complete blood count and blood iron levels, vitamin B12, folate, liver & kidney function tests.
- Urine tests – for detecting blood in the urine.
Your doctor will advise if you need further tests, such as:
- gastroscopy or colonoscopy – looking for signs of bleeding
- bone marrow biopsy
- faecal occult blood test – examining a stool sample for the presence of blood.
How Is Anaemia Treated?
Treatment depends on the cause and severity, but may include:
- Vitamin and mineral supplements, if you have a deficiency
- Iron replacement therapy if you are very low on iron
- Antibiotics if infection is the cause of your anaemia
- Altering the dose or regimen of regular medications, such as anti-inflammatory drugs if necessary
- Blood transfusions, if required
- Surgery to prevent abnormal bleeding, such as heavy menstruation
Note: Take iron supplements only when advised by your doctor. You could poison yourself if you take more than the recommended dose.
What Are The Preventions?
Some forms of anaemia can’t be prevented because they are caused by a breakdown in the cell-making process. Anaemia caused by dietary deficiency can be prevented by making sure that you eat food from certain food groups on a regular basis, including iron rich diet, dairy foods, lean meats, nuts and legumes, fresh fruits and vegetables.
Talk to your health professional if you are feeling unusually tired or if you follow a vegan diet (one that does not include any animal products).






What do you think?
You must be logged in to post a comment.